We Need to Maintain Funding for Biomedical Research: Witness CRISPR, CAR-T, and the Dark Genome
February 12, 2025

It’s a New Year and a new presidential administration in the U.S. Everyone it seems is making predictions, many dire, of what will happen in 2025. They are also looking back at progress made in recent years, trying to recommend what things we should preserve and what needs to be changed.
When we do this with respect to biomedical research we see many things that are nothing short of astonishing. Researchers continue to develop amazing new biomedical technologies that are creating promising new therapeutics. In our view, this progress clearly calls for sustained and even enhanced funding for the US research engines, the National Institutes of Health (NIH) and the National Science Foundation (NSF). Let’s look at just three such advances, CRISPR, CAR T, and the dark genome.
CRISPR Gene Editing
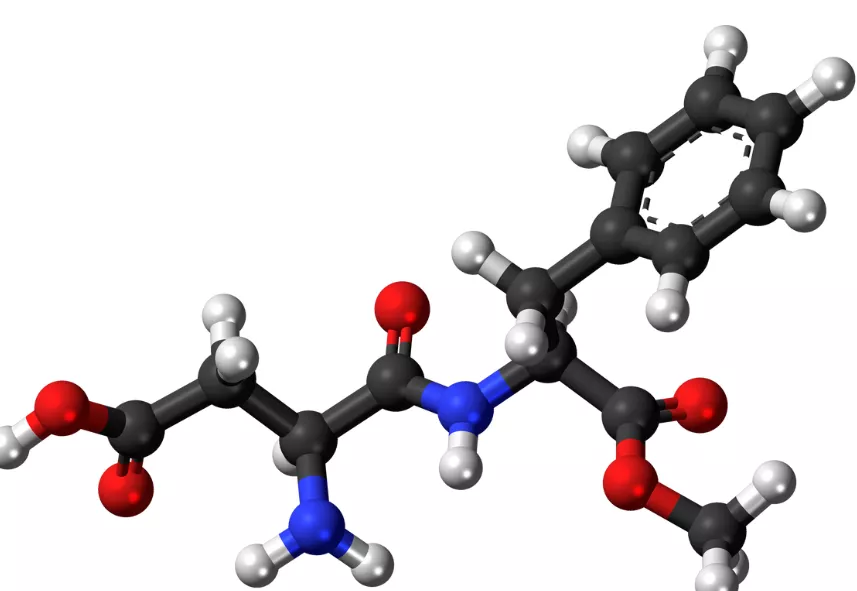
CRISPR (pronounced “crisper”) stands for Clustered Regularly Interspaced Short Palindromic Repeat. Now that is a mouthful, but here is what is involved. Around 40 years ago, scientists in Spain discovered that bacteria have a novel immunological method of fighting off invading viruses. The infected bacteria incorporate a small piece of the viral DNA into their own genomes and then generate a piece of RNA. When that virus again infects the bacteria, those RNA molecules recognize the viral DNA and carry along enzymes that destroy the virus. Using this information, scientists were then able to create RNA molecules that recognize sequences of human DNA in genes that they either want to turn off because they bear harmful mutations or turn on because they can be used to generate therapeutic proteins. These RNA guides are linked to an enzyme called Cas9 that can delete small pieces of DNA like a scissor. The process can delete a mutated gene that is causing disease or, in other applications of the CRISPR-Cas9 system, it is then possible to insert new DNA that will code for a beneficial protein.
CRISPR is only one approach to gene editing that is now making its way into clinical applications. In 2023 the first therapy using CRISPR, Casgevy, was approved for the treatment of sickle cell disease and in 2024 it was approved to treat another blood disease, beta-thalassemia. Both conditions are caused by a mutation in the gene that encodes for hemoglobin, the protein that carries oxygen in red blood cells to the organs of our bodies. In the case of sickle cell disease, a change in a single DNA base pair results in the creation of an abnormal form of hemoglobin, causing red blood cells to form crescent or sickle shapes in affected patients that clog blood vessels, causing extremely painful crises. Using the CRISPR-Cas9 system, Casgevy deletes a gene that causes the production of another form of hemoglobin to stop being produced shortly after birth. With the stop message deleted, this fetal form of hemoglobin is now produced again, compensating for the abnormal hemoglobin. A recent report showed that the benefits of Casgevy last for at least five years for patients with either sickle cell disease or beta-thalassemia. In that study, more than 90% of sickle cell patients had no painful crises for at least 12 consecutive months.
Casgevy is unsurprisingly not with downsides. To make the CRISPR-Cas9 system work, it is necessary to eliminate other blood stem cells using a chemotherapy drug called busulfan. This can cause infertility and even, as in one case in an investigational study, death. Another major problem with Casgevy is the cost, which is about $2.2 million per patient. Fortunately, scientists are now working on ways to deliver Casgevy without busulfan and to produce the drug in more cost-effective ways. Furthermore, they are vigorously pursuing applications of CRISPR for a host of other diseases, including autoimmune disease and HIV. All of this is incredibly promising, but it demands a high level of research funding.
CAR T To Destroy Cancer Cells
Another incredible advance is CAR T therapy for cancer. CAR T stands for Chimeric Antigen Receptor T-cell, again a mouthful. This therapy, already approved to treat certain forms of lymphoma, leukemia, and multiple myeloma, is a form of cancer immunotherapy. T cells are a type of white blood cell that circulate and play a key role in the immunologic response to infections. Each T cell has a receptor that recognizes a protein or antigen on an invading cell so that it can attach to it and play a role in its destruction. Cancer cells also bear unique proteins, and the goal of CAR T therapy is to engineer a patient’s own T cells so that they recognize these antigens and destroy the cancer cells. First, blood is drawn and T cells are separated from the rest of the blood. Then, these T cells are engineered in the laboratory to include a receptor that recognizes a specific antigen on the patient’s cancer cells. Finally, the newly engineered T cells are reinfused into the patient, allowing them to attach to and destroy cancer cells. The whole process takes about three weeks.
Intense research is now underway aiming CAR T therapy at other types of cancer, autoimmune disease, and other conditions. Once again, this approach is not without risks, and it is extremely expensive, ranging from $350,000 to over $500,000 for just the CAR T product itself, not including patient care costs. But once again, investigators are working to both reduce adverse side effects and to come up with methodologies that allow more cost-effective production of CAR T cells. The future is very bright for fighting cancer and other diseases with immunotherapy, but this will only happen if we maintain funding for basic and clinical research. We need to continue to support basic biomedical research because that is the engine that discovers the molecular and cellular targets for the therapeutic interventions we can then test in clinical trials.
The Dark Genome Opens Up New Therapeutic Possibilities
Many of us have heard about the mysterious forms of matter and energy in the universe called dark matter and dark energy. But how many know that scientists are also studying what they call the “dark genome?” We once believed that humans have more than 100,000 genes coding for the proteins that do the work in our bodies. But once the human genome was sequenced in 2003, we were surprised to learn that we have many fewer genes, perhaps, as was thought at the time, only between 20,000 and 30,000.
Now, however, that number is ramping up again. Traditionally, scientists stipulate that to be called a gene, a long stretch of DNA called an open reading frame (ORF) must be present that includes a signal telling a cell when to start and stop reading the gene in the process of coding for the messenger RNA (mRNA) that will ultimately be used to create new proteins. In the last several years, however, researchers have identified many shorter DNA sequences that nevertheless are transcribed to mRNA and result in the creation of short proteins consisting of only a few amino acids. It turns out that one of these short proteins is essential for the survival of abnormal cells present in a type of childhood brain cancer called medulloblastoma. Other short proteins may similarly be involved in promoting disease. Scientists believe we may have something closer to 50,000 genes and that the protein products of the dark genome may be involved in multiple forms of human illness. That means we will potentially have multiple new targets for disease interventions. Once again, that will only happen if we ensure these scientists continue to have adequate funding to do their work.
In an editorial in the journal Science last November, Sudip S. Parikh, CEO of the American Association for the Advancement of Science (which publishes Science), Marcia K. McNutt, president of the US National Academy of Sciences, and Dario Gil, senior vice president and director of research at IBM and chair of the National Science Board, lamented that the US share of global R & D declined 2 percent between 2010 and 2019, “while the rest of the world is catching up.” They warned that “the country risks ceding discovery and development—and their economic rewards—to nations that have plans to act and great will to invest. Even worse, scientific advancements will be slowed by a diminished US presence on the global science and technology stage.”
In highlighting CRISPR, CAR T, and the dark genome, we have only scratched the surface of the many marvelous achievements biomedical scientists are making. These advances promise to open many more avenues to treat previously intractable diseases. It is critically important that we bring this to the attention of our policymakers, who are understandably searching for ways to economize and reduce budget deficits. Nevertheless, cutting funding for biomedical research is not the right path to meet those fiscal goals. If anything, we need to increase research funding to sustain the remarkable progress that is already underway.
Related Posts

Two Events Affecting Women's Health Challenge Scientific Certainty
Posted in Cancer
Two recent reports related to women's health, one about breast cancer screening guidelines and the other about hormone replacement therapy, showcase how uncertain medicine can be.

Cancer Screening Does Not Always Extend Life
Posted in Cancer
Is cancer screening beneficial? Does it extend life? The evidence might be less clear than you think.
The Aspartame Saga
Posted in Cancer
Does aspartame cause cancer? An inside look at the recent debate after a WHO committee classified aspartame as a potential carcinogen.